Advocate Health
Mobilizing assets for health access and international development
Thursday, March 09, 2017
Friday, March 03, 2017
Synthesis of 2016 National Voluntary Reports at the High Level Political Forum
UN DESA champions efforts to enhance SDGs follow up and review at Incheon, South Korea
22 UN Member Nations reported in the first edition at the 2016 High Level Political Forum. At least 44 countries will be reporting on implementation status at this year's edition.
It is good to be back!
Thursday, March 25, 2010
A Brief Anthropology of the Nigerian Healthcare Tier System and Her Primary Healthcare Exigency: comments
Good (if slightly inaccurate) reading of Nigeria's medical history. Just wish to point out that the Colonial Medical Service started way before the Second World War. Indeed, the first set of medical officers were sent out in 1898. You are of course correct that primary attention was given to European personnel; but because part of the mandate of the service was to gather medical and scientific data, doctors had to be interested in treating locals.
You may wish to correct these in your blog so that some unknowing visitor may not be so misinformed.
Best wishes.
Thursday, November 12, 2009
Lessons from my trip
1. The destruction caused by the Liberian war is of no small dimension
2. The attendant national retrogression is not quantifiable
3. The human spirit is resilient
4. The efforts of the government here to return a similitude of normal life has reached a fevered pitch
5. The favourable disposition of the average Liberian towards Madam Ellen Johnson Sirleaf is contagious
6. The plea of Liberia for assistance with capacity building is urgent and cogent
7. There is a marked presence of the international community here helping with national revamping
8. The dearth of quality translational research in the West African sub-region is alarming
9. Feeble efforts are being made by stakeholders to correct this dearth
These are some of my thoughts.
Friday, October 16, 2009
Healthcare-Associated Infections
Hi IFEOLU
One thing everyone can agree on, no matter where they come down on the current health care debates, is that no one should get sick as a result of visiting the doctor.
Hospitals are rightfully expected to get you better but that's not always the case. Sometimes people are picking up infections, from pneumonia to antibiotic-resistant staph (MRSA), while under treatment for other health problems, or even while just in the hospital having a baby. That's a situation that could, and should, be completely avoidable.
Kimberly-Clark Health Care is on the forefront of protecting patients from Healthcare-Associated Infections (HAI) and has put together a site dedicated to that prevention called HAI Watch: Not on My Watch. The site has information for both healthcare professionals and healthcare consumers.
I would like to ask for your help getting the word out on AdvocateHealth!. Here's a microsite which explains everything. Please use any of the images, logos, videos, etc, on your site:
http://www.haiwatchnews.com/
Please let me know if you have any questions and if you are able to post, I'd really appreciated it if you'd send me the link.
Thank you,
Barbara
--
Barbara Dunn
barbara@haiwatchnews.com
www.haiwatch.com
Wednesday, October 07, 2009
Public-private partnerships for healthcare delivery in the African context: neologisms, sacrosanctity and the re-birth of Garki hospital.
Oral presentation.
FALEGAN Ifeolu Joseph. Consultant Family Physician, Garki Hospital, Tafawa Balewa Way, Area 8, FCT, Abuja, Nigeria. www.advocatehealth.blogspot.com. faleganji@yahoo.com.
The quest for efficiency and sustainability is beginning to impact healthcare delivery globally. There is a gradual departure from the norm. Public-private partnerships for healthcare delivery are being erroneously regarded as new entrants into the field of health systems reform. This axiom is being promoted in the parlance of world bodies in an attempt to improve health outcomes. However, healthcare delivery in every country involves some form of public-private partnership. In many countries where care is devolved through the public system, there is significant input from the private sector and vice-versa. This fact holds true for many African countries.
The public health system is decadent in a number of failed African states. The consequence is an unregulated private-driven healthcare system with a propensity for high out-of-pocket expenses in contradiction to the quality of care received. In Nigeria, for instance, close to 70% of healthcare is delivered by the private sector.
Garki hospital, Abuja, is the first acclaimed public-private partnership for health in Nigeria. The hospital was revived two years ago in a franchise that merged private finance initiative with government’s quest for quality healthcare delivery and has since then been dispensing care to patients from within and outside the Federal Capital Territory.
This presentation examines the different models of public-private partnerships in healthcare delivery drawing on examples from Spain, Australia, England, India and the Garki experiment. The presentation considers the advantages and disadvantages of public-private partnerships, the dichotomy between public and private initiatives and the key issues influencing performance such as competitiveness, cost, quality and flexibility. The implications of these especially as they relate to primary care and the practice of Family Medicine in resource-constrained settings are discussed.
Tuesday, September 08, 2009
Prostitution: social or spiritual problem?
Re: Prostitution is not a spiritual problem
By Osondu Anyalechi [oanyalechi@yahoo.co.uk]
Saturday, August 15, 2009
Dr. Ife Falegan, Consultant Physician at General Hospital, Abuja, was quoted in The Punch, July 24, to have said that prostitution is not a spiritual but a social problem caused by ‘lack of employment, accommodation, security and conducive environment’. This position assumes erroneously and absolutely that the drive to the cancer is money and if it is true, its cure must be money but is it always the case?
The desire for money to meet the needs he detailed above may induce a lady to join the trade but the compelling factor for most of them is certainly beyond money. A commercial sex worker confessed to me that she was deceived in Calabar by a lady who assured her of a job in Lagos. For the one-long week she stayed with her, the lady fed her and after that, initiated her into the profession. The victim said she did not know any place to go and had to join, making returns to the pimp - her commercial sex ‘godfather’.
But why didn’t she solicit for help from the Churches? A person who detests the trade may not end that way, even when all roads seem closed.
A divorcee joined the profession with the hope of making quick money with which to buy a sewing machine for making decent living. That ambition at the surface may look noble. But two, five and ten years, she was still in that business. With their charges of N 500 - N 1000 per customer and in a time of recession, ten patronizers a day is possible, could she still claim that she had not got enough money to meet that need? A few years ago, I brought five of them from Nwachukwu Drive to my office.
After ministering to them, I challenged them by tasking each of them to find her accommodation and my Church would sponsor her in any business or trade of her choice. It was painful that none of them took up the challenge. This debunks Dr. Falegan’s position about prostitution. It is certainly beyond money.
The problem is that most people define it narrowly, restricting it only to the single, giving the impression that married people are free from the mud. The lady in Proverbs chapter 7 was married. ‘Come, let’s drink deep of love till morning; let’s enjoy ourselves with love! My husband is not at home...’ What drives the venom goes beyond financial needs. Have drivers and houseboys, not been caught in bed with their Madams? Is the attraction to these lustful Madams money? How much did Joseph, a slave in Egypt and a houseboy to Portiphar, Pharaoh’s Captain of the Guard, have and to give her amorous and well-provided mistress? Have teenage school boys not been sexually harassed and abused by their school mistresses, old enough to be their mothers? Is it still all about money? I declare authoritatively that there is something in sexual perversion beyond what one lacks.
What do we call the practice whereby a lady, perhaps, a university student, who may not rent any apartment, but lives with her parents and hops from one man to the other? Some of these ladies are well-provided for by their rich parents, who are respected in the society. It is not only the children of poor parents that prostitute. In fact, if the census of virginity is conducted, most of the virgins might come from poor homes and not from the nobility. May we not also limit the practice to ladies as it is a malaise common to all genders.
If prostitution is a social problem, is armed robbery also the same? Are all the armed robbers from poor parents? Do we not hear how the children of the rich terrorize the society? There is a spirit behind prostitution and also armed robbery. What really prompts a man, married to a beauty queen, to be sleeping with his craw-craw-infested-mouth-stinking housemaid?
Why should a man leave his wife only to travel miles on end for an ugly lady even at the risk of his life? In agony, a wife told me that it would have been a different ball game if the lady was more beautiful than she. There was a man who was sleeping with a lady and in the midnight, he raped her baby that slept with them. Was it normal – a social problem? My wife ministered once to a prominent prostitute and she repented and dumped her foul profession and became a great tool in God’s hand. She was not given money but God’s Word. The unclean spirit was rebuked and it ran away. A lady in England was introduced to opium and the need of money to purchase the venom drove her to harlotry until the spirit was rebuked. She repented and became an evangelist.
If we give ten commercial sex workers one million Naira each, four of them may likely quit while the remaining six may continue. The same goes for armed robbers. There is of a truth, a social element in prostitution but the major element is spiritual. We met a lady in Tarkwa Bay who came for prostitution. We shared God’s Word with her and convicted by the Holy Spirit, she packed her stuff and followed us home. We gave her only her transport fare. Thus, it was not money but God’s Word that forced her out of the lion’s den.
Sunday, August 23, 2009
Hospitals for Humanity: 2009 Medical Mission Initiative to Africa
From the 6th to the 15th of December 2009, Hospitals for Humanity will be in Isanlu, Kogi State, Nigeria, on a Medical Mission Initiative to Africa to provide healthcare services to the people.
I put up this post so that you can adjust your schedule to free you to participate.
Please check the following link for details: www. hospitalsforhumanity.org.
Monday, August 11, 2008
A Brief Anthropology of the Nigerian Healthcare Tier System and Her Primary Healthcare Exigency.
Nigeria was colonized by Britain. Nigeria had no formalized planned health services until the end of the Second World War. Before the war, provision of health services was by the British Army Medical Services. The subsequent integration of the British Army and the colonial government gave birth to the Colonial Medical Service. The Colonial Medical Service provided free health services only to the British Army and the colonial service officers. Nigerians at that time only benefited incidentally. Nigerians were served primarily by a handful of mission and private hospitals sparsely scattered throughout the country.
In 1946, the colonial government promulgated a ten-year National Development and Welfare Plan. There was no separate national health policy at that time but the ten-year plan integrated all aspects of government endeavors, including health activities. The euphoria of independence, the devastation of the Nigerian civil war and the nuances of neocolonialism distracted Nigerian leaders after the expiration of the First National Development Plan. It was not until 1970 and 1975 respectively that the Second and Third National Development Plans were birthed. Although these subsequent development plans did not address the specific issue of a national health policy, the Basic Health Service Scheme evolved as part of the Third National Development Plan. The scheme attempted to put the semblance of a primary healthcare service in place. The scheme had the following objectives:
1. To increase coverage from 25 to 60 percent of the population receiving healthcare;
2. To correct the imbalance between preventive and curative medicine and in the distribution and location of health institutions;
3. To provide the infrastructures for all preventive health programs such as family health, environmental health, nutrition and control of communicable diseases; and
4. To establish a healthcare system best adapted to the local conditions and to the level of health technology.
The first national health policy was promulgated in 1988. The health policy content of the Fourth National Development Plan was in harmony with the first national health policy. At that time, the feverish agitation for Health for All by 2000 was at its peak worldwide. It was not surprising that the first national health policy set out to achieve health for all by 2000 through emphasis on primary health care.
At the moment, Nigeria has a three tier system of government comprising of local, state and federal governments. The Federal government at the center oversees the 36 State governments (and the Federal Capital Territory) and 776 Local Government Areas. The Local Government Areas are equivalents of districts in other countries. Each tier of government has its responsibility thus: the Federal Government oversees all health activities in addition to taking care of tertiary level healthcare at the Teaching Hospitals and Federal Medical Centers; the State Governments supervise health activities at the Local Government level and is solely responsible for secondary healthcare at the General Hospitals; and the implementation of primary healthcare has been devolved to Local Governments. The primary healthcare system is the first point of contact with the healthcare grid. The primary healthcare system in Nigeria is meant to ensure the:
1. Provision and maintenance of health infrastructure;
2. Planning and implementation of strategies to meet community health needs;
3. Provision of the ten primary healthcare components to the community;
4. Training of personnel and logistic support for community mobilization and participation; and
5. Management of health information system.
It should suffice to state that the Local Governments are presently ill-equipped to dispense the much needed primary health care to millions of Nigerians. In other developing countries, this bottom-up primary healthcare approach has successfully improved health outcomes.
Is it out of place to suggest that the government at the center should pay more attention to primary healthcare? Is it not true that the Federal Government has the most resources? Has it not been proven that improved primary healthcare delivery equates improved national health indices? Did Paul Farmer and colleagues not establish that sustainable quality healthcare delivery is possible even in resource-poor settings? Is it not true that most African governments scorn the promise to commit 15% of their budgets to health as contained in the Abuja Declaration? Have wealthy countries complied with the United Nations target of raising overseas official development assistance to 0.7% of their gross national product? Are the patents on medicines by developed economies not adversely affecting primary healthcare development in resource-poor settings? And is it not true that certain policy prescriptions by world bodies such as the World Bank and the IMF deter increased investments in primary healthcare?
These questions beg for answers.
Friday, March 07, 2008
Resolutions of the 51st National Coucil on Health Meeting: Further Responses
Evaluation of Niprisan (Herbal Medicine) for the Management of Sickle Cell
Anaemia
Charles Wambebe and Hadiza Khamofu, International Biomedical Research in Africa, Abuja, Nigeria, wambebe@yahoo.com, Joseph Okogun, Nathan Nasipuri and Karynius Gamaniel, National Institute for Pharmaceutical Research and Development, Abuja, Nigeria.
About 70% of all sickle cell anemia (SCA) subjects reside in Africa, estimated at over 12 million. The prevalence of SCA is estimated at over 2% while infant mortality is about 8% and survival rate of SCA babies in rural areas by five years of age is about 20%. These statistics indicate that SCA is probably the most neglected (and sometimes forgotten by health authorities) serious public health disorder with serious mortality and morbidity rates in Africa. The objective was to undertake pre-clinical and clinical assessments of a herbal extract vis-à-vis management of sickle cell anemia using Good Laboratory Practice and Good Clinical Practice principles respectively. In Africa, there is no standard treatment for sickle cell anemia, only palliative management is generally available. In view of this situation, most SCA subjects use herbal medicines. NIPRISAN is a standardized extract from four medicinal/food plants: Piper guineenses seeds, Pterocarpus osun stem, Eugenia caryophyllum fruit and Sorghum bicolor leaves. Short term toxicity study indicated that NIPRISAN was safe in laboratory animals. Bio-activity guided fractionation show that vanillin and aromatic aldehydes may be the bioactive moieties. NIPRISAN reversed sickled red blood cells and protected them from being sickled when exposed to low oxygen tension. NIPRISAN dose- dependently delayed polymer formation of haemoglobin S. NIPRISAN induced 85% increased solubility of deoxy haemoglobin S. The in vivo efficacy study was undertaken at Children Hospital of Philadelphia, USA. Histological examination of lungs of control Tg transgenic mice carrying human sickle haemoglobin showed entrapment of massive numbers
of sickled cells in alveolar capillaries. NIPRISAN significantly cleared the lungs of sickled cells. Furthermore, NIPRISAN induced profound effect on the survival time of Tg mice under hypoxic conditions (p<0.0001). The phase II clinical data indicated that all the subjects benefited from NIPRISAN with no serious adverse effect. About 80% of the subjects did not experience any crisis during the study (12 months). The subjects experienced significant reduction in hospital admission while attendance at school profoundly increased. Furthermore, there was no evidence of kidney or liver damage. NIPRISAN has been patented, licensed to an American company, registered and being manufactured at Abuja for global market.
Friday, February 08, 2008
Resolutions of the 51st National Council on Health Meeting: Responses
Dear Doctor,
why do you think it is at a conference so vital to the health of Nigeria that the development and use of Nicosan for sickle cell anemia is not even mentioned at this meeting?Here we have a drug that was developed by the Nigerian government and approved by NAFDAC but absolutely no urgency about getting it to the people who need it.The single mention of sickle cell comes with the only focus being the need for vaccinations in those people afflicted for influenza. Granted those people are at risk due to their physical state but that would not be the case if they were being treated with Nicosan.If Nicosan can return 50% of sickled cells to normal, improve the patient's health and end sickle cell crises would it not stand to reason that their health would be improved enough that they would not be at high risk for influenza?Why is the government not focusing on the distribution of a drug the Nigerian people have paid to develop and is good enough to be granted orphan drug status by the FDA and EU?What is wrong with Nigeria that almost 20 months after the approval of the drug that the government has yet to do anything about making this treatment available to the more than 4 million Nigerians who need it?The vast majority of deaths in childern under the age of 5 years born with sickle cell is not from influenza but from the genetic disease process itself. Focusing on influenza vaccines brought in from foreign countries vs treating the disease state itself with the indigenous drug Nicosan just doesn't make sense. If this is the approach Nigeria plans to take to meet it's Millinium goals of 2012 I am fairly confident they will fail. One of the most effective ways for Nigeria to reduce it's infant/maternal death rate would be to subsidize Nicosan distribution. So what's the government really doing when it chooses to support initiatives that preclude utilizing treatments that public monies have been spent to develop in favor of tertiary prophylactics like vaccinations? Vaccinations are not substitute for health. Prevention of infection does not come close to the benefits of treating the root cause of ill health. The Nigerian people should rise up and ask the government where the drug their tax dollars created is for them!
Posted by Anonymous to AdvocateHealth! at 4:47 AM
Tuesday, February 05, 2008
Resolutions of the 51st Nigerian National Council on Health Meeting
51st National Council on Health Meeting
Held at Planet One Entertainment Centre, Mobolaji Bank Anthony Way,
Ikeja, Lagos State, 21 – 23 November 2007
COUNCIL RESOLUTIONS
The 51st regular National Council on Health (NCH) meeting was held at the Planet One Entertainment Centre, Mobolaji Bank Anthony Way, Ikeja, Lagos State, 21 – 23 November 2007. A total of 732 delegates participated, from the Federal Ministry of Health and its Parastatals, State Ministries of Health and the Health & Human Services Secretariat of the Federal Capital Territory Administration(FCTA); and Development Partner Agencies which included WHO, UNICEF, DFID, the World Bank, AfDB, the Carter Centre. Delegates from the Health Regulatory Bodies, Military and Para-Military organizations also participated. The delegations from the Federal Ministry of Health, State Ministries of Health and the Health & Human Services Secretariat of the FCTA were led by the Honourable Ministers of Health, the Commissioners for Health and the Secretary, Health & Human Services Secretariat of the FCTA respectively.
2. The Council meeting was preceded by a two-day Technical Session held at the Aquatic Hall, Water Parks, Ikeja, Lagos State. It was chaired by the Coordinator, National Tertiary Hospitals Commission- Dr. Shehu Sule mni, who represented the Permanent Secretary, Federal Ministry of Health. The Technical Session was declared open by the Honourable Commissioner for Health, Lagos State.
3. The 51st meeting of the National Council on Health was declared open by His Excellency, the Executive Governor of Lagos State, Mr. Babatunde Raji Fasola SAN, who was ably represented by the Deputy Governor, Her Excellency Princess Sarah Adebisi Sosan. The Governor welcomed the Honourable Ministers, the Honourable Commissioners and the entire delegations to the NCH and expressed his appreciation, on behalf of the good people of Lagos State, for the opportunity given the State to host this most important meeting. He emphasized the importance of the National Council on Health Meeting to health development in Nigeria and restated the commitment of the Lagos State government to the attainment of the MDGs.
4. The Council meeting was presided over by the Honourable Minister of Health (HMH), Professor Adenike Grange. She welcomed the Council members and other delegates to the 51st National Council on Health meeting and expressed her pleasure at chairing the first meeting of the Council since assuming office. The Honourable Minister’s address focused on intimating Council with the vision and mission of her administration as well as obtaining the inputs and commitments of the Council members towards achieving the goal of “creating wealth through health” in line with the 7- point agenda of President Umaru Musa Yar’Adua that places a high premium on using Health and Education as the twin engine that drives national development by developing human capital.
5. The HMH in her address restated the strong commitment of the present administration to making Nigeria one of the top 20 economies in the world by 2020. This potential commitment has been buttressed by Goldman Sach’s team of global economists who identified Nigeria as having the potential to become one of the top eleven (11) economies in the world by 2020. She stated that although this goal was a laudable one, the poor health status of the people by whom the transformation would take place could impede its attainment.
6. The address also highlighted the fact that despite the existence of several effective and affordable technologies and interventions, gaps in health outcomes continue to widen due to a defective national health system. This situation continues to serve as an impediment to the achievement of the Millennium Development Goals (MDGs). Therefore, it is imperative to reposition and strengthen the weak and fragile health system to be able to deliver the services and high quality of care to those who need them in a timely manner, thus meeting the expectations of both the populace and healthcare workers.
7. The HMH recalled various reform programmes that had been commenced in the past leading to the development of several policies and strategic frameworks for various projects and programmes. However, these programmes have frequently not met their stated objectives due to inadequate emphasis on implementation, monitoring and evaluation. Hence the resolve of her administration to focus on the implementation of the developed policies and institutionalisation of mechanisms for monitoring and evaluation.
8. Other problems identified by the HMH include the loss of confidence in the primary health care sub-system and indeed the entire public health care system; obsolete or absent equipment and infrastructure; inadequate capacity of healthcare staff and training institutions; lack of a coordinated procurement and logistics system; lack of quality assurance or regulatory mechanisms for quality control; weak health information management systems; poor integration of health service delivery; and an almost non-existent referral system. She also reiterated the poor health and human development indices in the country and the threat these posed to the attainment of the MDGs.
9. The HMH solicited for the commitment of the Council members in the implementation of the National Health Investment Plan (NHIP) as a strategic approach to building consensus at all levels for the actualization of the Ministry’s vision. The NHIP will be implemented through six independent but related investment strategies which are: ensuring adequacy of policy instruments; resource mobilization and management; integrated disease management programmes; referral system and tertiary care development; increased surveillance; and full implementation of health insurance schemes.
10. She concluded her address by positing that greater investment in the health sector and more efficient and equitable use of resources are essential for national development. She appealed for greater collaboration between all tiers of government in the delivery of quality health services; and between policy-makers and technocrats in order to sustain the reforms while also suggesting to States to establish Primary Health Care Development Agencies to improve the delivery of primary health care.
11. The Honourable Minister of State for Health (HMSH), Arc. Gabriel Yakubu Aduku OON welcomed delegates to the 51st NCH meeting. He lamented the poor health indices of the country and opined that most of the causes of morbidity and mortality in the country could be effectively addressed at the primary health care level. The HMSH also seized the opportunity to once again buttress the seven (7) point development agenda of the present administration and especially Mr. President’s commitment to accelerating the achievement of the MDGs and improving the performance of the National Health System to one that is more adequately responsive to the health care needs of the people thereby enabling Nigerians live more economically productive lives.
12. HMSH therefore solicited for the support of the States in the translation of policies into actions and appealed for stronger commitment and a renewed synergy/partnership among stakeholders in the attainment of the MDGs. He concluded his address by charging all stakeholders in the health sector to join in the fight to eradicate malaria which has continued to be the leading cause of deaths among under-5 children as it is preventable and curable. He wished the Council fruitful deliberations.
13. In his address, the Honourable Commissioner for Health, Lagos State, Dr. Jide Idris, welcomed the Honourable Ministers, the Hon. Commissioners and all delegates to Lagos. He expressed his pleasure and that of the State for the opportunity granted them to host the 51st meeting of the National Council on Health. He emphasized the importance of effective health care to better health and the general development goals of a nation and hence the importance of the Council meeting where decisions at the Technical Committee meeting are analyzed for their merit before balanced policy decisions are arrived at for implementation.
14. The Honourable Commissioner went on to assert that due to the enormous resources required for the provision of effective health services, it was necessary for all tiers of government to be committed to investing heavily in health. He continued his speech by restating the commitment of the Lagos State Government led by His Excellency Mr. Babatunde Raji Fasola SAN the Executive Governor of Lagos State, to invest in infrastructure, human resources for health, provide adequate funding for the health sector, create systems, urgently address the issue of Maternal and Child Health as well as educate the public adequately. Lastly, on behalf of the State, he thanked all those present at the meeting and encouraged delegates to feel free to move around the State to see the different places of interest.
15. At the end of the opening ceremony, the vote of thanks was delivered by the Coordinator, National Tertiary Hospitals Commission, Dr. Shehu Sule mni, on behalf of the Permanent Secretary of the Federal Ministry of Health. He thanked the State Government and the people of Lagos State for the warm welcome and hospitality accorded all the delegates since their arrival in the State. This has no doubt encouraged the high quality of participation of the delegates in the meeting and would lead to the achievement of the purpose and objectives of the meeting.
16. After the opening ceremony, there were presentations on:
· Sector-wide, System-wide Implementation of PHC in Nigeria
By Dr. Kwame Adogboba
· The National Health Investment Plan and the role of States and LGAs in its implementation by Professor Adenike Grange, Honourable Minister of Health/Dr. Kenneth Ojo/Dr. Anthony Seddoh/Professor Wilfred Iyiegbuniwe
· Final Onslaught on Malaria in Nigeria by Dr. Yemi Sofola/Professor Kio Don-Pedro
· The Role of States Global Fund for AIDS, Tuberculosis & Malaria (GFATM) Activities by Professor Babatunde, DG,NACA
· Policy and Programme Implementation, Monitoring & Evaluation at Federal, State and LGA levels by Dr. Dan Onyeje; and
· Sector-wide Quick Wins and Indicators by Dr. Margaret Mafe
The presentation on Sector-wide, System-wide Implementation of PHC was followed by group discussions on various issues in the implementation of PHC. The following decisions were arrived at following the discussions:
· The need for the establishment of an agency in the health sector of the states that would be responsible for coordinating and facilitating the implementation of PHC;
· Integration of primary and secondary health care services with emphasis on decentralization of management;
· There should be pooling of funds from Federal, State and LGAs into “State Health Fund” for enhancing the management of health systems;
· The need to define and clarify the roles and responsibilities of governments and other stakeholders in the implementation of PHC;
· Promoting the implementation of the existing Public Private Partnership policy in health in Nigeria; and
· The establishment of a better and effective monitoring and evaluation system to monitor the performance of the health system at the state level
Council session was conducted in Plenary to deal mainly with the following:
i. Consideration and adoption of the Proceedings of the 50th National Council on Health (NCH/51/001) as amended.
ii. Report on the Implementation of Resolutions of the 50th NCH Meeting (NCH/51/002). Council noted the various stages of implementation of the 50th NCH meeting resolutions at the Federal and State levels and encouraged States to show more commitment by ensuring greater implementation of resolutions adopted at Council meetings. This could offer an opportunity for peer review and experience sharing.
iii. The recommendations of the Technical Committee which had earlier met on 19-20 November were reviewed.
17. After extensive and interactive deliberations, the National Council on Health approved the following resolutions:
PUBLIC/PRIVATE PARTNERSHIP FOR HEALTH
18. Council, noting the various efforts made by States in the implementation of Public-Private Partnership initiatives in the health sector as contained in the related Memoranda, commended the States that have started and encouraged all States to continue to explore the comparative advantage of PPP in health care delivery within the context of the National Policy on Public Private Partnership in Health.
STRENGTHENING PRIMARY HEALTH CARE SERVICES
19. Council, noting the critical importance of the PHC system in delivering quality health care to a large majority of Nigerians and the possibility of treating many of the leading causes of death at this level, appealed to States to establish State Primary Health Care Development Agencies as a strategy for enhancing the implementation of the PHC programme in their domains. The State PHCDAs could also serve as units for promoting, organizing and managing Public-Private Partnership initiatives in health in the States.
20. Council, noting the consistently poor health indices in the country, in particular, maternal, newborn and child health indices; and the inadequate human resource for health especially at the Primary Health Care level, approved the establishment of a Midwifery Corp Scheme for both basic and post-basic midwives to serve a compulsory one (1) year national youth service in the rural areas. Similarly, Council approved the compulsory posting of NYSC doctors to primary health care centres in the rural areas as a means of providing the necessary human resources for health at the primary health care level. Appropriate ancillary training in Life Saving Skills and Extended Life Saving Skills will be provided. The Council agreed on shared responsibilities between the three (3) tiers of government.
21. Council also approved the provision by the Federal Government of Midwifery Kits in Primary Health Care Centres for use by the midwives.
22. Noting the need to increase access to health care universally, Council approved the adoption of the Ward Minimum Health Care Package as a basis for the prioritization of health interventions, strategic and operational planning, budgeting, advocacy and resource mobilization by all stakeholders.
23. While noting the status of implementation of the construction and utilisation of model primary health care centres across the country Council appealed for better consultation with States, LGAs and Communities when siting PHCs.
STRENGTHENING SECONDARY HEALTH CARE SERVICES
24. Noting the poor quality of health care in the country, Council approved that a complete audit of the health care delivery system in all the States of the Federation should be undertaken with a view to identifying any weaknesses in the quality of care and implementing changes that may be required to assure high quality health delivery.
25. Council also approved the setting up of appropriate machinery for monitoring the provision of quality health care for Nigerians and encouraged States to develop friendly guidelines enshrining patients’ preference for the various outcomes with adequate budgetary provision for the implementation of these programmes.
26. Council noted and commended the construction of new and refurbishment of existing General Hospitals in Anambra State and the subsequent accreditation of these facilities for internship training by the relevant professional regulatory bodies.
FOOD AND DRUG ISSUES
27. Aware of the importance of availability of safe, qualitative and efficacious medicines for the effective functioning of any modern healthcare system; recognizing that lack of access to safe quality and affordable medicines is a major constraint to quality health care; realizing that lack of access to safe and affordable drugs has resulted in complications and even deaths; and considering that this situation cannot be allowed to continue if we are to achieve the MDGs:
28. Council considered a draft resolution which stated that “Council reviewed the drug distribution system in the country and noted that the system is still largely poorly coordinated leading to the proliferation of fake, sub-standard and unregistered drugs with its associated risks and therefore approved the establishment of legal drug distribution centres in all States and the FCT. Council further approved the government financing of the proposed nationwide assessment of government warehouses for lease or rent to the private sector for drug distribution.”. After deliberations, it was decided that the issues entailed required more consultations before consensual decisions could be reached. The draft resolution was thus stepped down.
29. While noting that one of the goals of the National Drug Policy is to stimulate increased local production of essential drugs as well as ARVs and ACTs and the target to produce 70% of national drug needs by 2008, Council approved government’s financing of the proposed nationwide assessment of the capacities of local drug manufacturing industries in order to derive current data on local drug production.
30. Also, in a bid to boost local drug production, Council made a commitment to resist pressure to lift the ban on drugs listed on the 2005 import prohibition list and to upgrade the list based on data that would be generated from the nationwide drug production assessment exercise. Council would also revisit the issue of high tariffs on imported pharmaceutical raw materials while considering other incentives for local drug manufacturing companies.
31. Council noted the benefits of an effective drug revolving fund scheme and commended States in which such schemes have been functioning and sustained while encouraging other States to replicate the schemes.
MATERNAL, NEONATAL AND CHILD HEALTH
32. Council noted with concern the rather slow progress made towards reducing maternal, newborn and child mortality midway to the target year for the attainment of the MDGs, due to poor access to high impact, evidence-based, cost effective interventions and approved the adoption of the Integrated, Maternal, Newborn and Child Health (IMNCH) Strategy developed by the Federal Ministry of Health and partners as a strategy to promote a more holistic, comprehensive, integrated approach to maternal, newborn and child health issues and services as well as the accelerated scaling-up of programmes to reach the target groups.
33. Noting the issues and programmes affecting the health of the mother and child and all the efforts made by the federal and state authorities as contained in the related memoranda, Council commended states for their efforts to improve the health status of women and children and to reduce morbidity and mortality indices among them; however, Council encouraged them to integrate these services in order to maximize the utilization of available resources and achieve the greatest possible impact on the health of the people.
34. Taking cognizance of the proven benefits of Misoprostol in the control of post partum haemorrhage; its ease of administration and relatively few dose-dependent side effects, Council approved the inclusion of Misoprostol in the essential drugs list as part of efforts to reduce maternal morbidity and mortality.
35. Council reviewed and adopted the final draft of “Gender-Based Violence in Nigeria: National Guidelines on Prevention and Response” and encouraged all States and the FCT to approve, adopt and implement the recommended strategies.
36. Re-emphasizing the benefits of exclusive breast-feeding for newborns and taking cognizance of the challenges posed to working mothers in implementing the strategy, Council encouraged all workplaces in Nigeria to provide well equipped and staffed crèches for their female employees as these could also be very important catchment sites for routine immunization. Council also encouraged the Ministries of Health, Women Affairs and Labour & Productivity to work together to plan and implement reproductive health education and counseling programmes for women workers.
DISEASE CONTROL
40. Concerned about the increasing magnitude and public health importance of noncommunicable diseases(NCDs) and their risk factors; the absence of programmes focusing on NCD control in the states, and the need to scale up NCD prevention and lifestyle and behavior change campaigns to check the increasing burden of NCDs; Council resolved that all states should as matter of priority, establish or strengthen and fund appropriately an integrated NCD prevention and control programme in the state and LGAs, coupled with the designation of a state focal point for NCD control. The FMOH will provide technical support to improve state capacities in the development, implementation, monitoring and evaluation of NCD programmes.
41. Acknowledging that blindness is a major cause of unnecessary human suffering, often leading to poverty, social exclusion and early death; and aware of the poor coordination of the commendable work undertaken by voluntary/ non governmental Organizations (NGOs) in the control of blindness in Nigeria, Council resolved and approved that the National Vision 2020 Strategic Plan be adopted as a policy document for implementation at the tertiary, secondary and primary levels of health care services, for elimination of the main causes of avoidable blindness by the year 2020. All the Governments should develop 5 year action plans for Eye Care Services within the context of the National Vision 2020 framework and strengthen inter-sectoral collaboration in the implementation of these plans.
42. Committed to the plan to eradicate Guineaworm by December 2008; noting the need for improved budgetary allocation and timely disbursement of funds required at the LGA, State and Federal levels and the need to intensify surveillance activities for the successful implementation of the last phase of guineaworm eradication; Council resolved that action should be accelerated by all tiers of government and all relevant agencies in the provision of safe water especially in the rural communities; recommended the intensification of Community Participatory Surveillance Strategy; and integration of guineaworm surveillance activities with other grassroot health programmes
43. Concerned about the plight of sickle cell patients and Nigerian children who are both plagued by Pneumococcal and Hib infections; noting that safe effective Haemophilus Influenza type B (Hib) and Pneumococcal Vaccines are available and already being used effectively in our neighboring countries, Council approved that the Federal Ministry of Health works out ways to provide the vaccines for use in the country starting with sickle cell patients who need them most.
HIV/AIDS
44. Council noted the, and commended the National HIV/AIDS and STI Control Programme, for the successes achieved in previous sentinel surveys and the States for their efforts in the control of HIV/AIDS.
45. Further noting the importance of HIV/AIDS sentinel surveys in the determination of prevalence and distribution of HIV infection, sensitization of stakeholders to take appropriate action in prevention and control of the epidemic, planning, implementation and monitoring of HIV/AIDS programme and also for assessing the overall impact of the interventions by stakeholders in the control of HIV infection; Council recommended that the Federal Ministry of Health should facilitate easier access to World Bank’s credit funds and states should make available sufficient budgetary provisions to ensure that they can play agreed roles in the conduct of 2007 survey and future surveys.
MALARIA
46. Recognizing that malaria still remains a major cause of morbidity and mortality especially amongst children and pregnant mothers; considering the limitations of our past efforts towards the elimination of malaria; and realizing the need to accelerate the elimination/eradication of malaria in Nigeria through the implementation of an integrated approach which should include Integrated Vector Management (IVM) strategy; Council resolved that all governments should embrace the new approach for malaria control/elimination/eradication which is the integration of the RBM (Roll Back Malaria) and IVM interventions, and adopt year 2015 as the target year for the total elimination of malaria from Nigeria
HUMAN RESOURCE MANAGEMENT
47. Council noted the dynamic nature of medical knowledge and practice and thus the need for every medical officer to be exposed to new knowledge and discoveries in his/her area of specialization in order to assure the quality of healthcare delivery; and recommended that all Governments should support continuous professional development of all healthcare workers; and MDCN should promote and make efforts to institutionalize continuous professional development (CPD) as a pre-requisite for registration and licensing.
48. Council deliberated extensively and agreed on the effect of variations in salaries paid to health workers across the country on their motivation and efficiency of the healthcare delivery system. Council resolved that a forum should be set up by the FMoH and States to deliberate and agree on a harmonised salary scale for health workers in order to address this problem.
49. Council appreciated the proposed National Health Investment Plan and recommended that the Federal Ministry of Health plays the leading role in its development while states and all other relevant stakeholders would participate and cooperate as appropriate . Some of the expected outcomes of the implementation of the National Health Investment Plan will be to: increase political support for increased budgetary allocation to health and other health investments; enhance coordination and efficiency in the use of donor assistance; develop and implement comprehensive strategies for achieving effectiveness, efficiency and equity of the health sector; provide a basis for better result-oriented budgeting in the health sector; ensure the efficient and equitable utilisation of available health resources; provide an objective framework for monitoring and evaluating the health sector; and improve the overall functioning of the health system for national development.
INFORMATION MEMORANDA
50. A total of seventeen information memoranda were considered by Council. Further to receiving and deliberating on them, Council commended and noted all the memoranda. The information memoranda are:
· Development of National Health Investment Plan
· Establishment of the National Tertiary Hospitals Commission (NTHC)
· Establishment of the National Centre for Disease Control (NCDC)
· International Health Regulations (IHR) 2005
· The Establishment of Field Epidemiology and Laboratory Training Programme (FELTP) in Nigeria
· Traditional Medicine Development
· Presidential Committee on Pharmaceutical Sector Reform
· National Chemical Safety Management in the Health Sector
· National Drug Fomulary/Essential Drugs List (NDF/EDL) Review Committee/Secretariat-DFDS
· Progress Report on National Food Risk Analysis Centre in NAFDAC
· Baseline Study carried out by NAFDAC on the quality of Medicine in circulation in Nigeria
· Progress Report on the Health Systems Development Project II
· NHIS the Journey so far as at October, 2007
· Establishment of Functional Traditional Medicine Boards
· Anambra State Community Health System and Health Financing Scheme
· Dutch Government-assisted Community Health Insurance Scheme in Kwara State SHONGA, BACITA, PILOT STUDY/SCHEME
· The Lagos State Health Facilities Monitoring & Accreditation, Journey so far
· Avian Influenza Control and Human Pandemic Preparedness and Response in Nigeria
51. The 52nd National Council on Health meeting is scheduled to hold in Kano State in May, 2008.
52. The 51st National Council on Health meeting was declared closed by the Honourable Minister of Health, Professor Adenike Grange at 2.17 p.m. on Friday 23 November 2007.
Thursday, November 08, 2007
Healthcare Financing in the Developing World: Is Nigeria’s Health Insurance Scheme A Viable Option?
The idea of a National Health Insurance Scheme was first considered by the authorities in 1962 but successive governments lacked the political will to actualize this dream. It was not until 43 years after when the immediate past President, Chief Olusegun Obasanjo, set apart the sum of 26 billion Naira for the scheme in the 2005 budget. The former president directed at that time that no deductions be made from any government employee until the end of 2006 when the performance of the scheme would have be evaluated. He opined that this grace period would allow for confidence building. His speech at the launch of the program in June 2005 attempted to debunk the widespread cynicism been exhibited by majority of Nigerians about this typical Nigerian white elephant project.
The Nigerian National Health Insurance Scheme (NHIS) was established by Decree No 35 of 1999. The Decree states that “there is hereby established a scheme to be known as the National Health Insurance Scheme (in this Decree referred to as "the Scheme") for the purpose of providing health insurance which shall entitle insured persons and their dependants the benefit of prescribed good quality and cost effective health services as set out in this Decree”.
The NHIS decree statutorily allows each insured person to decide which health centre he wishes to register with. A monthly capitation is paid to the health centre from the pooled funds. Health Maintenance Organizations (HMOs) are empowered to coordinate the activities of the health centers as they dispense healthcare to the insured while the over-all regulation of the scheme rests with the National Health Insurance Scheme Council. The council was established by the same decree.
The WHO has this to say about healthcare financing in Nigeria: “Funding Health in Nigeria is from a variety of sources that include budgetary allocations from Government at all levels (Federal, States and Local), loans and grants, private sector contributions and out of pocket expenses. The value of private sector and out of pocket expenditure contribution to financing the sector is yet to be determined. According to a World Bank source, the public spending per capita for health is less than USD 5 and can be as low as USD 2 in some parts of Nigeria. This is a far cry from the USD 34 recommended by WHO for low-income countries within the Macroeconomics Commission Report. Although Federal Government recurrent health budget showed an upward trend from 1996 to 1998, a decline in 1999 and a rise again in 2000, available evidence indicates that the bulk of recurrent health expenditure goes to personnel. Federal Government recurrent health expenditure as a share of total Federal Government recurrent expenditure stood at 2.55% in 1996, 2.96% in 1997, 2.99% in 1998, declined to 1.95% in 1999 and rose to 2.5% in 2000. Beyond budgetary allocations, a concern in funding the health sector in Nigeria is the gap between budgeted figures and the actual funds released from treasury for health activities”.
The Nigerian NHIS is already facing some problems. Some segments of the populace are left out. Recently, retired senior citizens complained on national television that the scheme does not cater for them. There is the issue of integrating the rural populace who do not have clearly identifiable sources of income since their means of livelihood is mainly subsistence farming. There is also the problem of inadequate human capacity to drive the NHIS. There is still a dearth of necessary professionals grounded in healthcare financing whose input cannot be done away with. And how will the NHIS survive if we do not deal squarely with the recurrent problem of graft? And graft manifests in different ways: from the healthcare provider who does not make essential medicines available or provides poor quality service, to the HMO who deliberately delays/withholds captitation. Many of the consumers grapple with the bottlenecks associated with accessing healthcare under such an administratively cumbersome scheme. Perhaps the greatest problem facing the NHIS is the monopoly it enjoys as lack of competition stifle growth and birth mediocrity. The success recorded in the telecommunication industry in Nigeria so far has been attributed in part to the vigorous competition it is experiencing. Many are already calling for the liberalization of the health insurance business as obtainable in some developed economies.
The foregoing clearly lends credence to the fact that for sustained development in the healthcare industry in Nigeria and the developing world, healthcare financing must not be left in the hands of government alone; certainly not in the hands of inept, pathologic, corrupt governments. It is in this vein that many have proposed other funding options including the somewhat ‘extreme’ idea of wrenching the NHIS from the hands of government lest it goes the way of other public enterprises such as the National Housing Fund, National Provident Fund, and many defunct Pension Schemes.
We should begin to promote the commercial health insurance option as this will bring some life into the health insurance industry in the developing world. Informal prepayments arrangements as is the case with some rural cooperative societies such as Country Women Association of Nigeria (COWAN) have been proposed as an attractive model for low income urban/rural populations in the informal sector since this eliminates the high cost of premiums necessary to subscribe to commercial health insurance. The downside to this model is that the fee-for-service approach may compromise the quality of service provided by healthcare providers. It is also very likely that the amount contributed by these poor families may not be adequate to cater for major illnesses.
Before the developing world finds her feet, donor countries/agencies can explore the possibility of setting up not-for-profit Voluntary Health Insurance Plans (VHPs) which has great potentials for mitigating the numerous health problems of the poor.
Wednesday, November 07, 2007
Paul Farmer: The Man Who Would Cure The World
The Pulitzer Prize-winning author, Tracy Kidder, described Paul Farmer as "a man who would cure the world". I found the following brief bio about Dr Farmer on Harvard Medical School's website: "Medical anthropologist and physician Paul Farmer is a founding director of Partners In Health, an international charity organization that provides direct health care services and undertakes research and advocacy activities on behalf of those who are sick and living in poverty. Dr. Farmer’s work draws primarily on active clinical practice (he is an attending physician in infectious diseases and chief of the Division of Social Medicine and Health Inequalities at Brigham and Women’s Hospital (BWH) in Boston, and medical director of a charity hospital, the Clinique Bon Sauveur, in rural Haiti) and focuses on diseases that disproportionately afflict the poor. Along with his colleagues at BWH, in the Program in Infectious Disease and Social Change at Harvard Medical School, and in Haiti, Peru, and Russia, Dr. Farmer has pioneered novel, community-based treatment strategies for AIDS and tuberculosis (including multidrug-resistant tuberculosis). Dr. Farmer and his colleagues have successfully challenged the policymakers and critics who claim that quality health care is impossible to deliver in resource-poor settings".
I consider him a great inspiration.
Friday, November 02, 2007
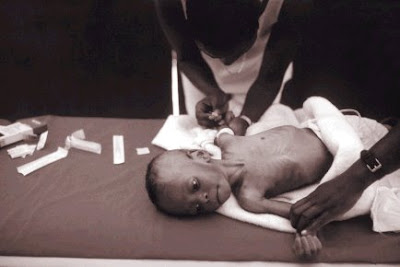
Caesarean Birth at Evangel Hospital
ECWA Evangel hospital trains Family Medicine residents to dispense care and solve common health problems that are common to most people in most places with the most cost-effective approaches. The ability to be able to rapidly carry out a Caeserean delivery is one of the fundamentals of emergency obstetric care. The video is one of several deliveries carried out regularly by the highly competent personnel at Evangel Hospital. Take a peep!
Just rearranged this blog!
Post your comments/suggestions about this to my mailbox. Thanks!
Friday, October 05, 2007
The Millennium Development Goals: counting down to 2015
In September 2000, 189 Heads of State adopted the UN Millennium Declaration. It was a roadmap setting out goals (Millennium Development Goals) to be reached by 2015. There are eight goals, 18 targets and 48 indicators to measure the MDGs. Three out of the eight goals and eight of the 18 targets relate directly to health. These are:
· Goal 4: Reduce child mortality
· Goal 5: Improve maternal health
· Goal 6: Combat HIV/AIDS, malaria, and other diseases.
Targets related to the goal of combating HIV/AIDS, malaria, and other diseases are:
· Have halted by 2015 and begun to reverse the spread of HIV/AIDS
· Have halted by 2015 and begun to reverse the incidence of malaria and other serious diseases.
How far have we gone down the road towards achieving these goals with just eight years left to that all-important deadline?
There has been some progress. However, nearly 11 million children under the age of five die every year globally. In 16 countries, 14 of which are in Africa, levels of under-five mortality are higher than in 1990. More than 500,000 women die in pregnancy and childbirth each year and maternal death rates are 1000 times higher in sub-Saharan Africa than in high income countries.1
A growing awareness of malaria’s heavy toll, matched with a greater commitment to curtail it has helped to spur key malaria control interventions, particularly insecticide-treated net use and access to effective antimalarial drugs. Resistance has now developed to all classes of antimalarial drugs except artemisinin and its derivatives. When used correctly in combination with other antimalarial drugs, artemisinin is nearly 95% effective in curing malaria. The rationale is that when two drugs with different modes of action are given simultaneously they attack different targets in the parasite. If a mutation should occur to make the parasite resistant to one of the drugs, the second drug will kill it.
In just four years (1999-2003), distribution of insecticide-treated mosquito nets increased 10-fold in sub-Saharan Africa. Despite this progress, urban dwellers are six times more likely to use the nets than their rural counterparts, according to data available from a number of countries in the region. Similarly, the richest fifth of the population are 11 times more likely to use them than the poorest fifth.2
There were an estimated 8.8 million new tuberculosis (TB) cases in 2005, including 7.4 million in Asia and sub-Saharan Africa. More than 1.6 million people died of TB, including 195,000 patients infected with HIV. The number of new tuberculosis cases is growing by about 1% per year, with the fastest increases in sub-Saharan Africa. More ominous has been the emergence of extensively drug resistant tuberculosis (XDR-TB).1, 3, 4
Fortunately, it has not been all doom and gloom. Recently comes a World Bank Report which states that the AIDS pandemic is on the decline in countries such as Rwanda, Uganda and Ethiopia. The infection in West Africa has not reached the high levels it was feared that it might reach. It cannot also have been bad that the recently concluded G8 summit at Heiligendamm, Germany promised $60 billion dollars to combat the spread of HIV/AIDS and other diseases affecting Africans.
Certainly with the right combination of commitment and aid, there is still enough time to achieve the Millennium Development Goals.
1. United Nations Department of Economic and Social Affairs. The Millennium Development Goals Report 2006; New York, United Nations June 2006.
2. Year in Review 2006. Geneva; World Health Organization 2007.
3. Global Tuberculosis control: surveillance, planning, financing. WHO report 2007. Geneva, World Health Organization, 2007 (WHO/HTM/TB/2007.376)
4. Raviglione MC, Smith IM. XDR Tuberculosis- Implications for Global Public Health. N Engl J Med 2007; 356 (7): 656-9.
*Dr. A. Onu is of the Department of Family Medicine of the Jos University Teaching Hospital and Editor-in-Chief of the Jos Journal of Medicine. This piece is the editorial of the current issue of the Journal. I am an Associate Editor of the Journal.
Tuesday, September 18, 2007
Where AIDS Efforts Lag
By Lola Dare, Jim Yong Kim and Paul Farmer
President Bush made a historic pledge in his 2003 State of the Union address: to get urgently needed AIDS
treatment to 2 million people living with HIV in impoverished countries by 2008. Congress concurred and
launched a major initiative to fight AIDS focusing on 15 developing nations. At a U.N. General Assembly
conference on AIDS this year, the United States went further and committed, along with other countries, to come
as close as possible to universal access to HIV treatment by 2010.
We have come a long way since 2000, when AIDS treatment was available to only the fortunate few. Activists
campaigned successfully to drive down the cost of treatment with affordable off-patent AIDS medicines that are
now available in most developing countries. After initial objections, the U.S. government became a major
purchaser of generic drugs.
But now that donor governments are providing more funding and medicines are becoming available, a new
bottleneck threatens the success and sustainability of the effort. People with AIDS in Africa are dying simply
because there aren't enough nurses, doctors and pharmacists to administer treatment. Without a new effort to
train, retain and support health workers in numbers sufficient to meet basic needs, the United States will not be
able to keep the deal it made with Africa in 2003.
It takes years to graduate a new doctor or nurse, and most of them prefer to build a career in a major city with
well-equipped hospitals. But with modest investments, donor governments can quickly empower and mobilize an
army of health workers made up of the hundreds of thousands of unemployed or underemployed people living in
the very settings where HIV's toll is heaviest. Women in particular are often already serving as caregivers at the
community level, usually without training or compensation.
Starting in Haiti's central plateau, the organization Partners in Health has trained and employed hundreds of
accompagnateurs, or health companions, across the group's projects in five countries, including the United States.
Accompagnateurs are paid a stipend to provide a broad range of services, including drug distribution, disease
observation and reporting, clinical referrals, and the social support that people with chronic illness so often need.
This modest investment is, we believe, one of the chief reasons that adherence to AIDS therapy is so high within
our projects -- and why death rates are so low.
Community health workers are lay people on the front lines who provide effective health services and support in
countries reeling from AIDS. These nonprofessionals -- often living with HIV themselves -- are rooted in their
communities, can be trained quickly and are less likely to emigrate in search of better wages and working
conditions. They have deep knowledge of their communities, where they are familiar and trusted neighbors. With
continuing training and support, they can rapidly form a strong and active force filling deadly gaps in health
personnel and services.
Many programs have sought to rely on "volunteers" and deny these laborers pay for their services -- a model
conceived in wealthy countries. But in poor countries this amounts to exploitation of the poorest to treat the
sickest. It should be replaced by programs that ensure living wages, continuing training and a career path.
Community health workers cannot succeed alone; they are not an excuse to cut corners. Professional backup
from doctors, nurses and medical officers is necessary to provide supervision and to treat referrals. But the pool
of available health professionals in many African countries is too small to address basic primary-care needs and
far from adequate to supply new donor-sponsored global health programs.
Unintentionally, the laudable U.S. efforts to fight AIDS and malaria in Africa can end up weakening primary
health systems that are already crumbling by hiring doctors and nurses away from public clinics and hospitals
where they are also desperately needed. When primary public health systems fail, disease-specific initiatives will
also fail. The United States must get serious about increasing the overall supply and retention rates for health
professionals in sub-Saharan Africa.
According to World Health Organization estimates, the U.S. share of the global cost of training and supporting a
healthy workforce sufficient to meet internationally agreed-upon targets in sub-Saharan Africa is roughly $8
billion over five years.
On this World AIDS Day, we must match the audacity of President Bush's 2003 pledge with a complementary
initiative for training and keeping enough new health professionals and community-level workers to fulfill the
promises the United States has made.
Article from The Washington Post, Friday, December 1, 2006; Page A29
Lola Dare is executive secretary of the African Council for Sustainable Health Development International. Jim
Yong Kim and Paul Farmer are co-founders of Partners in Health International; both teach at Brigham and
Women's Hospital and Harvard Medical School.
Tuesday, September 11, 2007
Tales from West Africa

Her lexical prowess will bow you over! You will also discover that she is not afraid to be vulnerable as she blogs from the heart.
You can access the blogs at http://www.jankwanomedic.blogspot.com/ andhttp://www.saralynnnege.wordpress.com/
Thursday, September 06, 2007
Winning the War against HIV/AIDS: Involving Community Health Workers
Several studies have already established the place of CHWs in the war against HIV/AIDS. I stumbled on a WHO document recently which is a must-read for everyone involved in this war.
We can no longer wait for PLWHA/PABA to come to us. We must go into the community and look for them. We must be proactive. And we cannot do this effectively without the CHWs.
Please read the WHO's document on CHWs at this link www.who.int/whr/2004/chapter3/en/index5.html
Tuesday, July 17, 2007
Dr Tom Thacher goes to Mayo Clinic
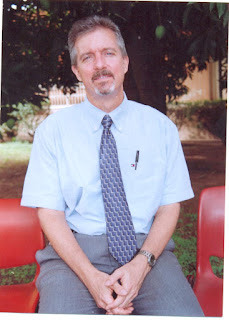 I thought about this post for a while before writing. I especially was concerned about the fact that Tom may not approve. Yet, I found it difficult to resist the urge to write about a man who is many things to many people. I eventually came up with a short write-up, adopting a middle-of-the-road approach.
I thought about this post for a while before writing. I especially was concerned about the fact that Tom may not approve. Yet, I found it difficult to resist the urge to write about a man who is many things to many people. I eventually came up with a short write-up, adopting a middle-of-the-road approach.In an earlier post, I discussed the importance of the discipline of Family Medicine as the panacea to the problem of health access in resource-poor settings suggesting the need for a paradigm shift from heavy spending on tertiary institutions to increased budgetary allocation to ensure sustainable primary care development. I had earlier raised the issue of inadequate human capacity, among others, pointing out that for resource-challenged settings to succeed in their bid to improve their health outcomes, they must train and retain healthcare workers who will not only dispense quality primary care but also embark on research that directly impart the people and provide patient-oriented evidence that matters.
There is someone who has played a key role, albeit quietly, in the forgoing for the past 20 years in Nigeria. He is Dr Tom Thacher.
He came to Nigeria as a missionary after completing his residency in Family Medicine in the United States about 20 years ago. He established the department of Family Medicine and Informatics at the Jos University Teaching Hospital after working in some other centers. He started with the training of four residents but at the moment, there are 25 residents in the department. Many of the early residents have graduated and either gone on to become trainers in other centers or taken up positions of responsibility in Nigeria’s health industry.
Tom was the director of research at the Jos University Teaching Hospital. He provided guidance for specialists in other disciplines and supervised residents’ dissertations. He conducted groundbreaking studies in rickets and researched into common killer diseases such as malaria, tuberculosis and HIV/AIDS. I read a copy of a Liverpool University PhD thesis on tuberculosis he supervised. He insists that research done in any community should impart the people.
Tom promoted the place of medical informatics. He recently supervised the creation of a database for entry of all patients’ data seen at the department of Family Medicine of the hospital. The department attends to more than 35,000 patients annually.
Tom is strict and disciplined. Pasted in a conspicuous place in his office is this inscription: “Your lack of planning is not my emergency”. He is an avid reader and a time manager. He leads by example, something rare in this society. We who followed had no option than take a cue. He is content, never showy, almost austere. In spite of his many achievements, his published papers, his pedigree, he remained simple, humble.
He insists on excellence. He supervises my dissertations for the faculties of Family Medicine of the West African College of Physicians and the National Postgraduate Medical College of Nigeria and demands no less from me.
Dr Tom Thacher’s life in Nigeria cannot be fully elucidated here: it is for another place, for another time.
He now joins faculty at the prestigious Mayo Clinic in Rochester, USA.
Thursday, April 12, 2007
The Emergence of XDR Tuberculosis: Implications for Public Health in Resource-limited Settings.
XDR tuberculosis, classified as cases that are resistant to three or more of the six second-line drugs for the disease, has a mortality rate of more than 85%. This is not altogether a new occurrence as XDR tuberculosis was first described more than a decade ago.
XDR tuberculosis is not the same as multi-drug resistant (MDR) tuberculosis. In the latter, Mycobacterium tuberculosis has become resistant to isoniazid and rifampicin.
South Africa is at the moment trying to contain an outbreak of XDR tuberculosis which has spread to all the country’s provinces. The WHO is sending a permanent staff to that country to help with the containment effort. The resistant strain of the Mycobacterium tuberculosis is said to have originated from the KwaZulu-Natal province. Experts are of the view that XDR tuberculosis has spread beyond South Africa citing the lack of adequate diagnostic capacity and poor notification mechanisms as the reasons why the outbreak is being under-reported by other countries. Mario Raviglione, director of Stop TB at WHO refers to the outbreak as an absolute emergency lamenting that the world is not responding quickly enough. A US$95 million dollar appeal made in Paris last October to combat this emerging threat has met little response.
We all know that the very existence of XDR tuberculosis is an indictment on our health systems since it reflects weaknesses in tuberculosis management which otherwise should minimize the emergence of resistance. Early, accurate diagnosis and timely institution of the appropriate curative regimen which are monitored for adherence are important steps in tuberculosis control. When drug regimens and tuberculosis control are sub-optimal, drug-resistant strains are selected which eventually proliferate and with repeated treatment errors, multi- and extensively-drug resistant strains are born.
Chances are that in most resource-poor settings, the scenario I painted above about tuberculosis management and inefficient health systems is often the rule rather than the exception. It follows then that if the status quo remains, tuberculosis might go beyond what we now know as XDR tuberculosis.
There is no easy panacea to this threat. But the panacea does exist; we must be ready to pay the price. Who wants to experience the torment of tuberculosis becoming an incurable disease?
Resource-poor settings need an effective disease control infrastructure beginning with strengthened rapid diagnostic capacity which is accessible and can be deployed at the point of care. This should be supported with unlimited access to quality first- and second-line drugs with mechanisms put in place to ensure adherence. Preventing spread is a challenge but it is doable. Special attention needs to be paid to the immune-suppressed patients because of their vulnerability. All HIV patients should be screened regularly for latent tuberculosis and antiretroviral drugs should not be delayed unnecessarily. As a matter of urgency, resource-poor settings must have access to drug-susceptibility testing which at the moment is mainly found in developed societies. The place of increased surveillance and research bordering on TB control cannot be overemphasized. And I suggest we hurriedly form enduring partnerships designed to urgently enhance the production of third line drugs which the world is taking lightly now.
Monday, March 26, 2007
In the Spirit of the Doha Declaration
How come then Novartis instituted a lawsuit against a company in India for producing generics of the anticancer drug, Glivec? The generic costs about $2,700 yearly per patient while Glivec costs $27,000 for the same time period.
Pfizer is fighting the Philippines government for approving a generic of the antihypertensive, Norvasc. The generic costs 90% less.
Oxfam International released a report recently stating that rich countries have broken the spirit of the Doha Declaration (see www. Oxfam.org for a copy of the report, Patents versus Patients: Five Years after the Doha Declaration). The report states that many wealthy countries go to great lengths to protect medicine patents putting profits before patients. As a result, patented medicines continue to be priced out of the reach of the world’s poorest people.
It is instructive to remember that the burden of disease continues to rise especially in poor countries. For instance, between 2001 and 2005, more than 4 million people became newly infected with HIV in developing countries. Yet, 74% of AIDS medicines are still under monopoly, 77% of Africans have no access to AIDS treatment and 30% of the world’s population does not have access to essential medicines.
In the spirit of the Doha Declaration, the Oxfam report concluded with some recommendations which I agree with and summarize in my own words below:
1. Wealthy countries should live up to their promise and relax the strict intellectual properties laws as regards patented medicines.
2. Rich countries should muster the political will to provide technical support that will enhance universal access to essential medicines
3. Leaders in developing countries should become responsible and explore, with a view to invoking, the “public health safeguards written into the WTO’s intellectual property rules” in order to abolish differential access to medicines.
4. Pfizer and Norvatis should, if not in the spirit of the declaration, for the sake of corporate social responsibility, end their feud with developing countries.
Thursday, March 22, 2007
His Excellency’s ludicrous Elixir for AIDS
I was flustered by the claims being made. I still am.
His Excellency, the President of the Gambia, Yahya Jammeh, had invited the CNN team to come and see the wonders being wrought by an herbal concoction he had personally formulated for the treatment and cure of AIDS. The constituents of the concoction were revealed to him in a dream!
Many Gambians have already abandoned their HAART for this miracle cure and the risk for resistance will certainly skyrocket because many antiretroviral agents are unsparing.
CNN’s repeated efforts to interview the president failed and attempts to subject the concoction to standard scientific testing met a brick wall. An expatriate who spoke out against the president’s farcical claims was thrown out of the country within 48 hours. Even more disheartening is the fact that the health minister, a physician trained in the West, swore on set that the concoction can cure AIDS.
What is wrong with Africa?
Why has his Excellency forgotten so soon similar claims made by Thabo Mbeki and the former South African health minister? Did his Excellency ever hear of Nigeria’s Dr Abalaka? Why return to ideas and claims that belong in the Stone Age? Why belittle the threat of a scourge currently devastating us, the world’s poor? Why would the Gambia, a country with a Medical Research Council which is home to prolific, world-renowned researchers drag Africa backward in her quest to see the end of AIDS?
Why?
Thursday, February 22, 2007
Meet Ron Brittan

Few legal practitioners there are who render services for free. And we cannot castigate those who charge fees: it is just the way things go; commerce, among others, drives society.
Certain individuals, however, have gone above the norm, above our basic human egocentric tendencies. Such individuals extol our communality. Such persons, like Ron Brittan, possess large hearts.
I refered a friend who was in dire need of legal assistance to Ron recently who rendered help promptly, free of charge. This same gesture he has extended to other acquaintances in the past, rationalising that this is his modest contribution to bridging inequality and promoting equity for poor communities.
Ron Brittan, a legal practitioner, immigration activist and social worker who resides in Oxford, England, wrote the following lines to me recently..........."Dear Joseph:
I checked out your blog and found it extremely interesting. I wish you every success in achieving your noble objectives.
I too am concerned with the Millennium Goals, especially as far as Nigeria is concerned. I try to make a small contribution by assisting young people to come to UK to study, and to get work experience, so as to return to their country with enhanced skills. Your friend Andrew is a case in point.
Most of our leads come from Rotary and Rotaract clubs in Nigeria, through a programme initiated by the Oxford Rotary Club. Notably, many members of Jos Rotaract club have participated.
Hope to hear from you again, and we may possibly be able to pool some ideas.
Ron Brittan,
Immigration Link (An Oxford charity)".
His webpage www.geocities.com/ron_brittan/index.html is even more revealing.
This post is an ode to Ron!


